The Explanation of Benefits (EOB) is how the payer communicates with the clinic once the claim has gone through the adjudication process. The EOB is extremely important as it tells the clinic what the insurance is paying and provides the reasoning behind the decision. An EOB can help direct the biller on how to resolve the additional balance through write-offs, patient payments, or secondary insurances. The EOB can arrive as a paper document or electronically as an 835 ERA file.
The following questions are answered in an EOB:
- What client is the payment for?
- What is the Date of Service?
- What CPT codes were paid?
- How much did the insurance pay?
- How much was adjusted?
- How much is owed by the client?
- What is the reasoning for the payment/adjustment amount?
Sample EOB
Let’s review this example explaining how to read an EOB’s detail page. Please note that detail pages can be several hundred pages in length.
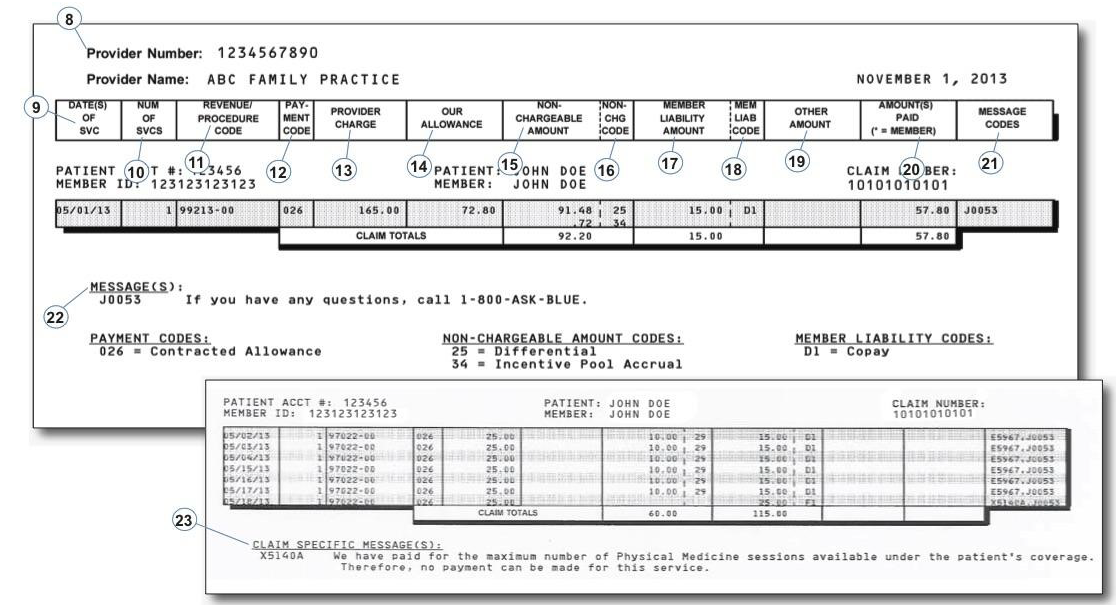
- Billing Provider’s NPI
- Date(s) of Service
- Units for the specific CPT code
- CPT Code
- Codes that describe the type of pricing on the claim
- Original Charge Amount
- Allowed Amount (Contracted Rate) for each the specific CPT code
- Adjustment Amount
- Code that describes why the provider cannot charge the client the amount in field 15
- Client Responsibility Amount
- Code that describes why the member is liable for the amount in field 17
- Other payment amounts (i.e. other insurance payments)
- Amount paid to the Billing Provider, unless the payment is made to the client. Payments made to the client are denoted by an asterisk (*)
- Codes that correspond to the messages at the bottom of the Detail pages.
- Claim messages
- Additional claim messages

Comments
0 comments
Article is closed for comments.