When you submit an electronic claim, an 837 EDI file is created and sent to the corresponding clearinghouse. After that, the system is not in control of your claim. Fortunately, the application has tools in place to help make sure your claims are processed.
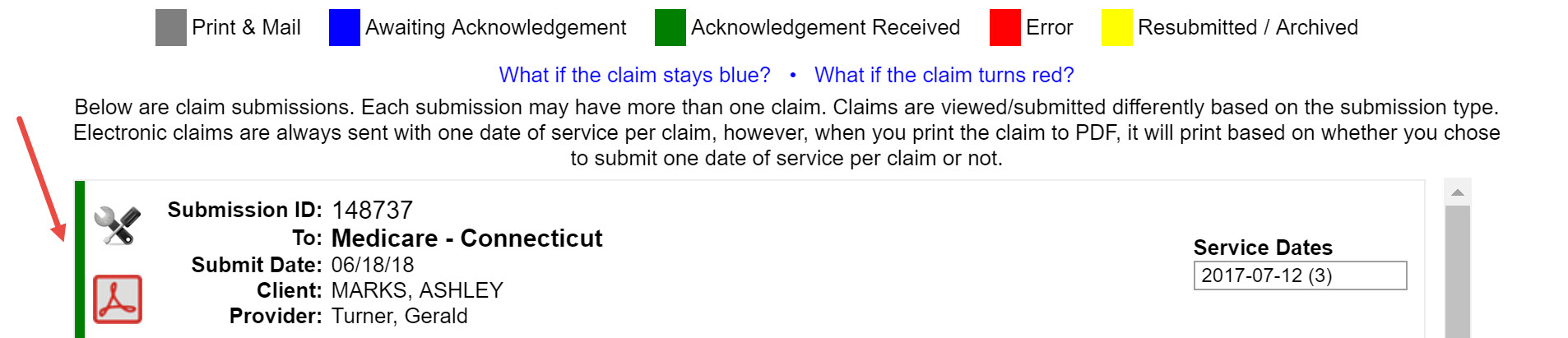
Color Coding
The Filing > CMS-1500 area indicates the status of each claim by placing a colored bar to the left of each claim. Every message sent by the clearinghouse or payer has the ability to change the color of the bar.
![]()
- Gray - Claim was created as Print & Mail
- Blue - Claim was created as electronic and submitted
- Green - Claim was received by either the clearinghouse or payer
- Red - Claim was rejected from the clearinghouse or payer
- Yellow - Claim was resubmitted or is considered to be old
Acknowledgment of Receipt
When a clearinghouse receives the claim (837 file), they send back a 999 Acknowledgement receipt. This does not mean that the claim will be accepted and processed by the payer. Upon receipt of the 999 file, the system will change the color bar in the CMS-1500 Filing area to green.
After the clearinghouse receives the claim, they scrub the claim and either forward it to the payer or send a rejection message back to your account. When the payer's EDI department receives the claim, it is scrubbed even further. The payer will send a 277 (payer response) file that either contains an acceptance (green) message or a rejection (red) message.
What if the color code on my claim stays blue?
Acknowledgments are usually sent within 1-3 days of submission. If you have the Unacknowledged Claims alert turned on, you will receive a notification on your dashboard if a claim has been blue for more than 5 days. If the claim has been blue for a prolonged period of time:
- Call the payer and check on the status. You are doing this to see if they received the claim and failed to send back an acknowledgment. This will help to reduce duplicate claims.
- If the payer states that they have not received the claim, then you will want to resend the claim. To resend a claim, click the
 icon associated with the claim and select Resend Electronically.
icon associated with the claim and select Resend Electronically. 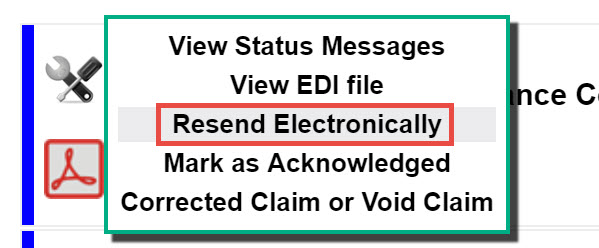
The claim is blue but I have verified that the insurance company does have the claim
If you have verified that the payer has received the claim, then you can manually acknowledge the claim. To mark a claim as acknowledged, click the ![]() icon associated with the claim and select Mark as Acknowledged.
icon associated with the claim and select Mark as Acknowledged.
Error
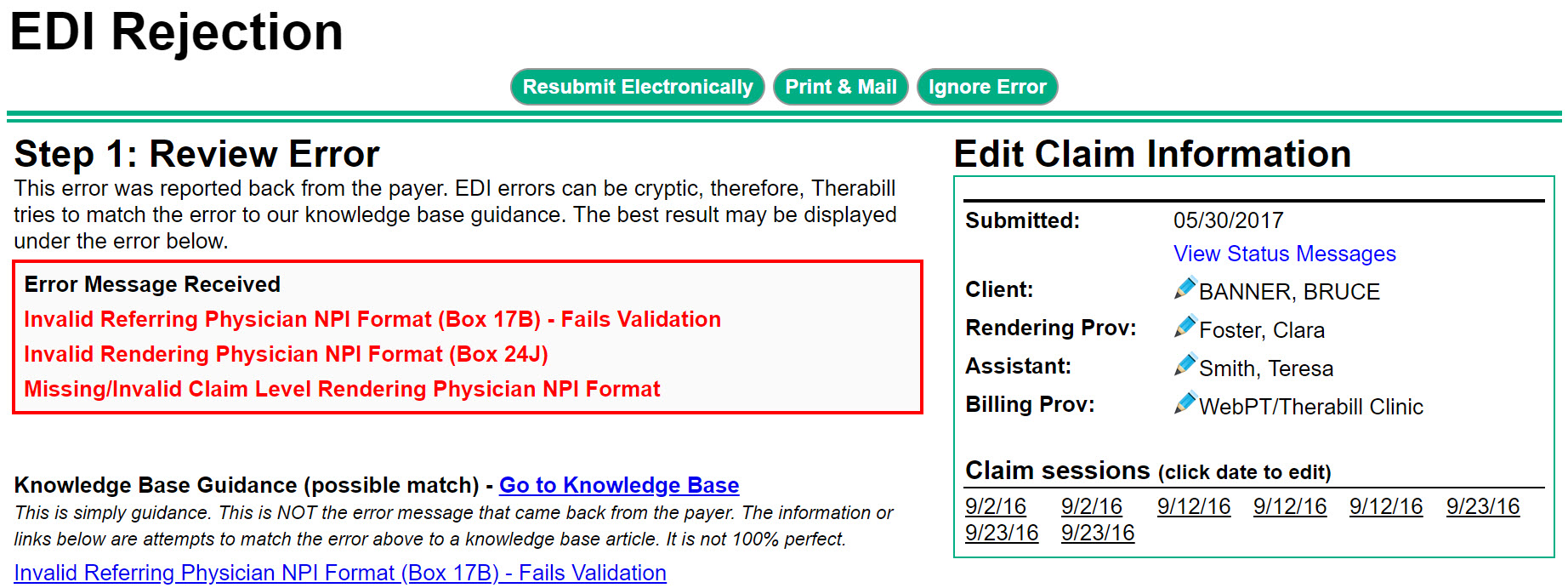
If the clearinghouse or payer rejects the claim, the bar will turn red to indicate an error. Additionally, an entry will be created on your dashboard under Electronic Claim Errors.

Each entry will display the client name, the insurance the claim was invoiced to, and the date the claim was rejected. When you open a rejection, information will be displayed that details the rejection, the claim information, and often times, links to articles that can help you correct the errors.
Making sure you are getting paid
Remember, the green bar simply means that the claim was received. It is not an indication that you should or will receive payment. To make sure you are getting paid:
- Look out for the Unacknowledged Claims alert (if turned on) and Electronic Claim Errors.
- Ensure that you are entering all payments and adjustments that you receive from payers and clients. This is the only way to know that the reports within the system are accurate.
- Frequently access your Balance Aging Report and follow up on your older claims that are still outstanding.

Comments
0 comments
Article is closed for comments.