Value of element SBR01 has been already used in loops 2000B/2300. Elements SBR01 are expected to be different from SBR01 specified in loop 2000B and to have unique values within loop 2300 excluding \'U\' value. Segment SBR is defined in the guideline at position 2900. Invalid data: P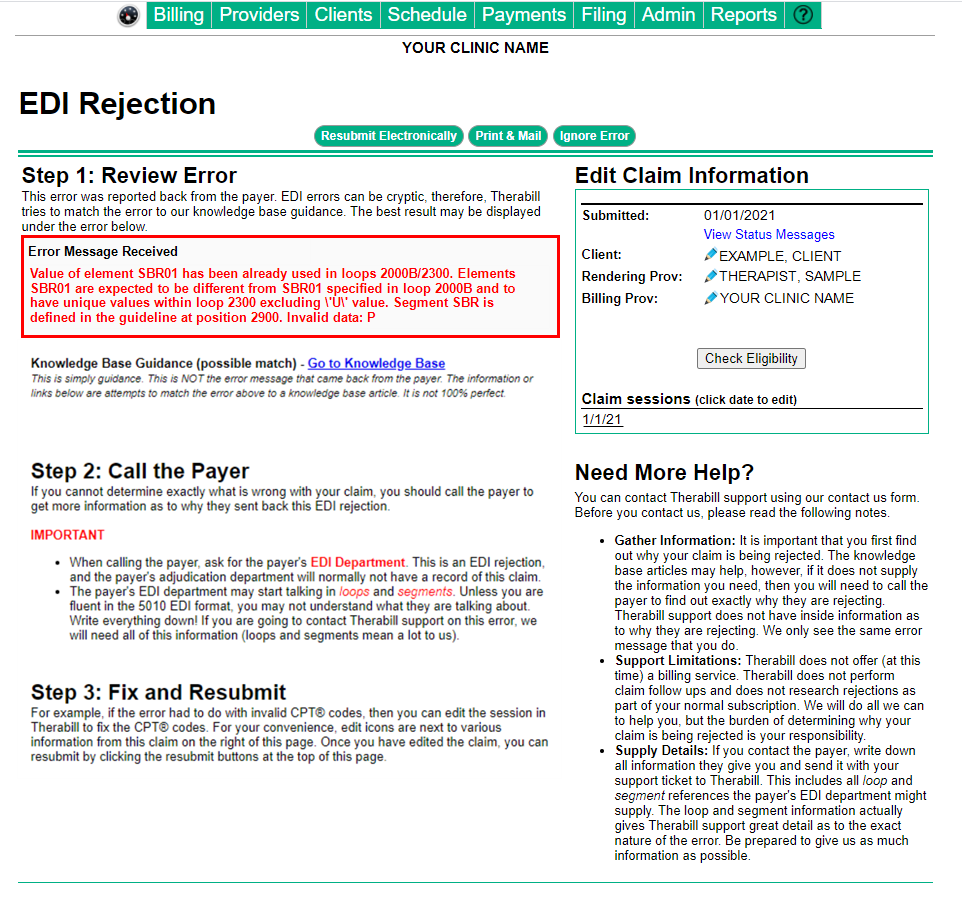
This error indicates erroneous payments/adjustments are attached to the claim. When sending secondary claims there should only be one payment and one adjustment listed in the payment history.
To Resolve
Remove the erroneous payments/adjustments attached and re-enter the payments/adjustments once the claim has been submitted.
Remove Payments
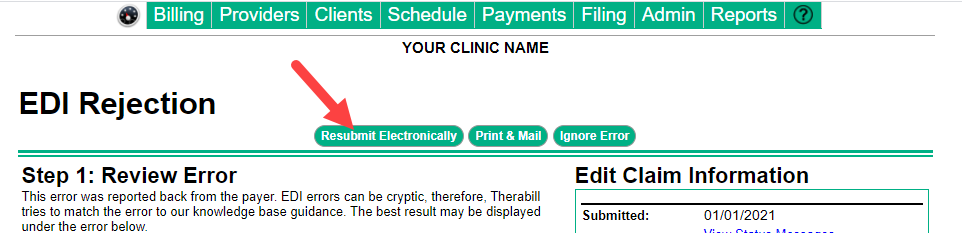
- From the Edit Claim Information section of the EDI rejection page, click the
 (blue pencil) next to the client’s name.
(blue pencil) next to the client’s name.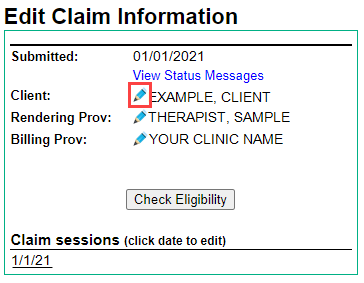
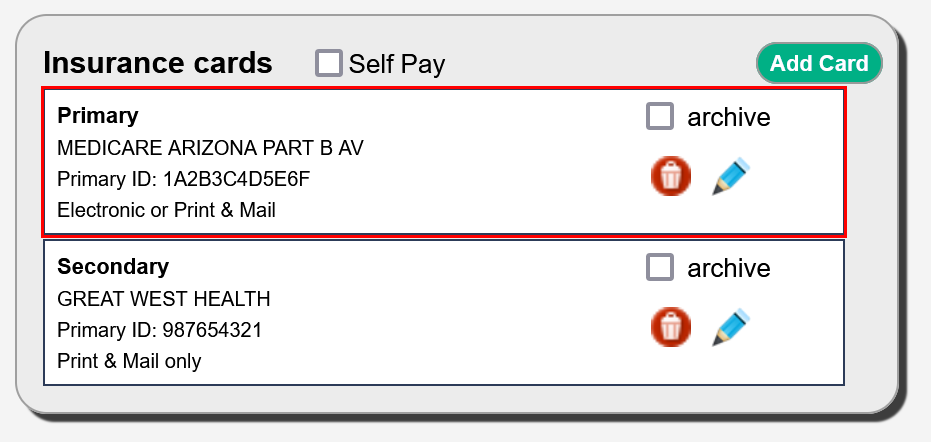
- Review the insurance cards under the Billing Info section and note the Primary Insurance listed.
- Exit the patient chart, then from the Edit Claim Information section of the EDI rejection page click on the affected Date of Service (DOS) under Claim Sessions.
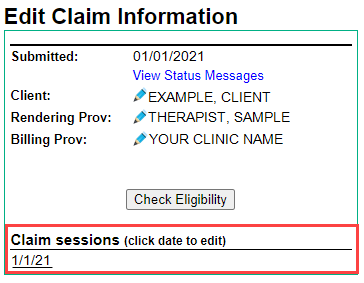
- Then click the
 (black dollar sign) to open the session.
(black dollar sign) to open the session. - From the Payment History section, use the
 (delete) button to delete any payment from the posting session that does not come from the Primary Insurance. A secondary payer claim should contain only one payment and one adjustment or each CPT code from the primary payer, any other payments and adjustments must be removed for the secondary payer to accept the claim.
(delete) button to delete any payment from the posting session that does not come from the Primary Insurance. A secondary payer claim should contain only one payment and one adjustment or each CPT code from the primary payer, any other payments and adjustments must be removed for the secondary payer to accept the claim.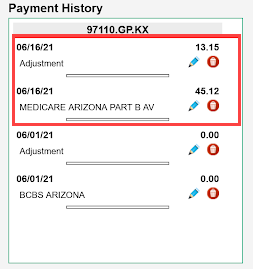
- Once all the incorrect payments and adjustments have been removed, you can exit the session by clicking the
 (red x) in the top-right corner of the page.
(red x) in the top-right corner of the page. - Resubmit this claim from the EDI rejection page by clicking Resubmit Electronically.
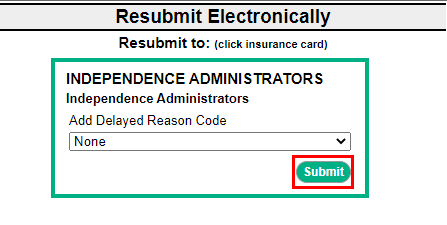
- To confirm resubmission, click Submit.

Comments
0 comments
Article is closed for comments.