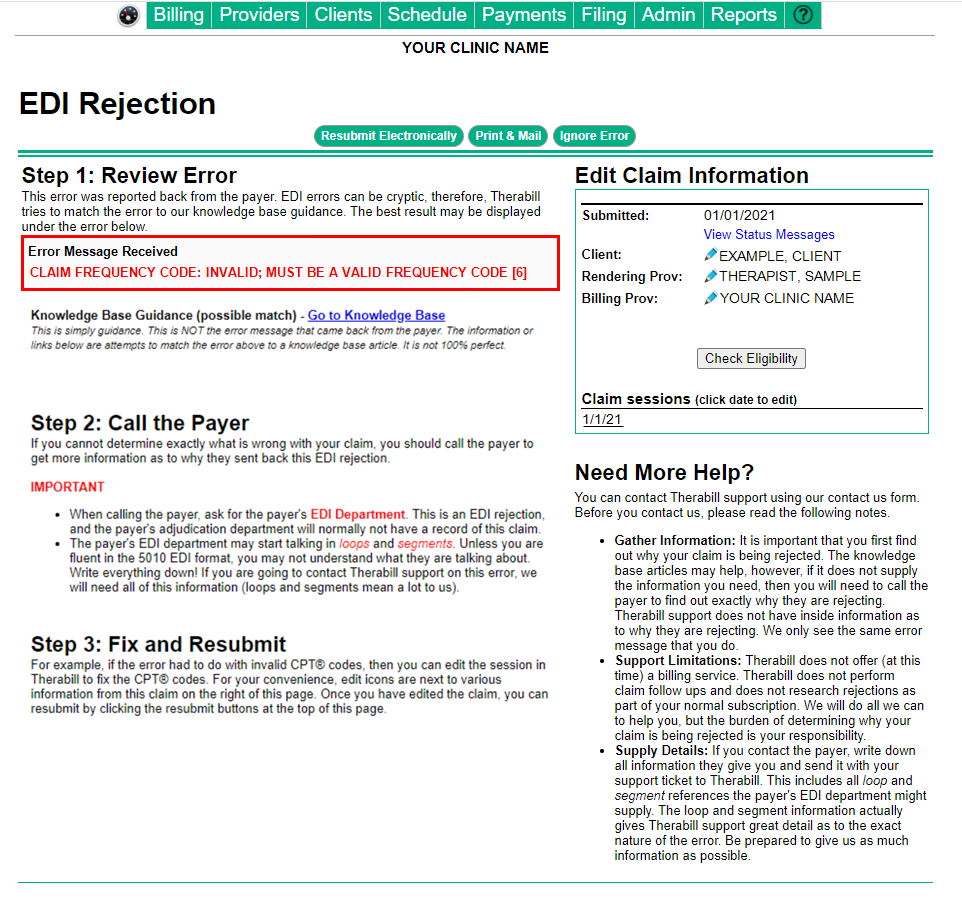
This error occurs when using the Claim Frequency Code 6 for the payer. The payer claim frequency code is a code on the electronic (EDI) claim that indicates if the claim is an initial submission, voided claim, corrected claim, etc.
The claim was most likely submitted as a corrected or voided claim and the code that was used to create the corrected/voided claim is not accepted by this payer.
To Resolve
Follow the steps below to file a corrected claim using Frequency code: 7 and resubmit the claim.
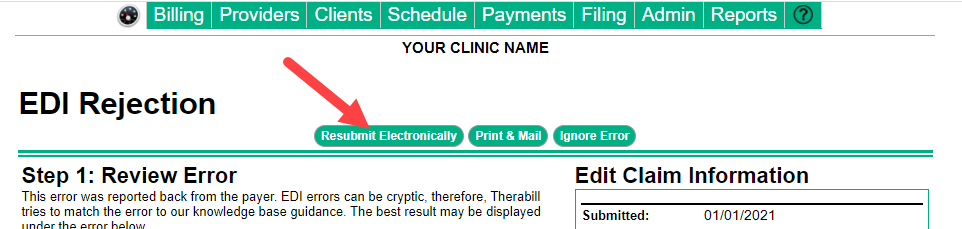
Move the claim to the Bill Insurance Invoicing area
- From the Edit Claim Information section of the EDI rejection page click on the affected Date of Service (DOS) under Claim Sessions.
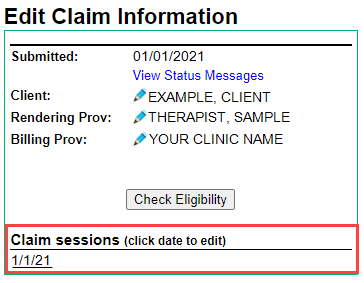
- Then click the
 (black dollar sign) to open the session.
(black dollar sign) to open the session.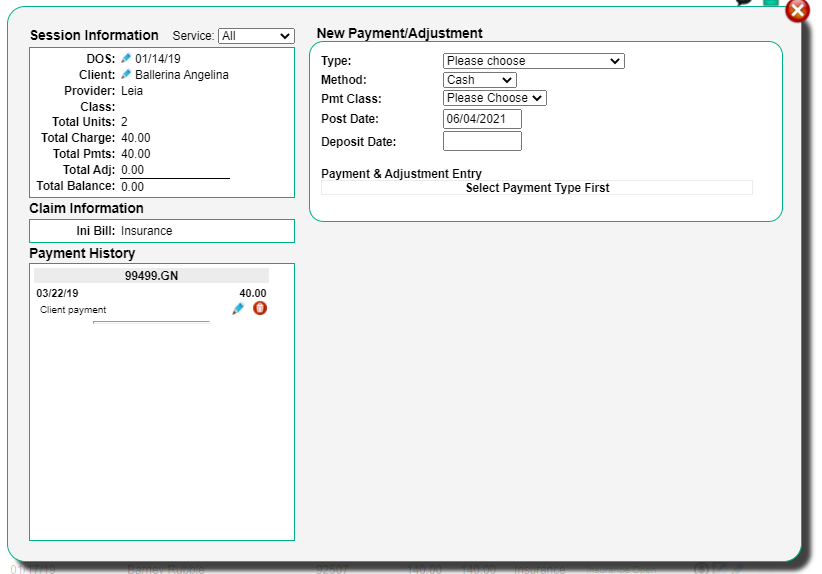
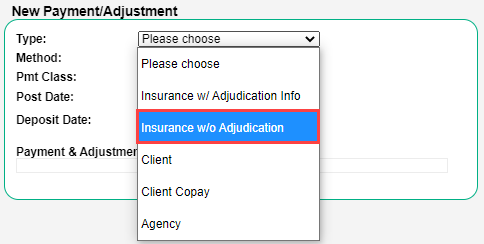
- Use the Type drop-down in the New Payments/ Adjustments section and choose Insurance w/o Adjudication Info.
- From the Payment & Adjustment Entry Section Enter 0 for the New Pmt amount.
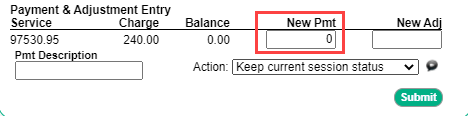
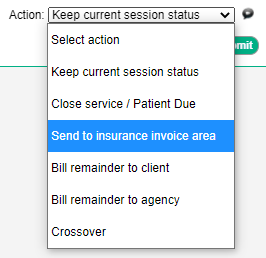
- Use the Action drop-down and select Send to insurance invoice area, then click Submit.
Electronic Corrected Claims
After placing the claim in the Bill Insurance Invoicing area.
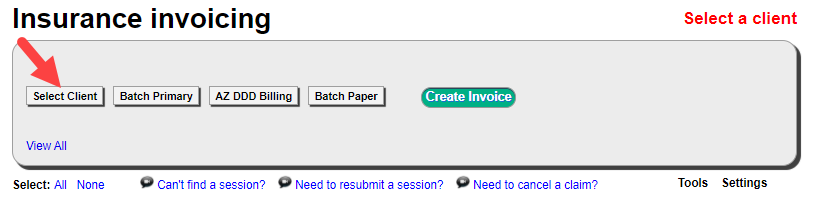
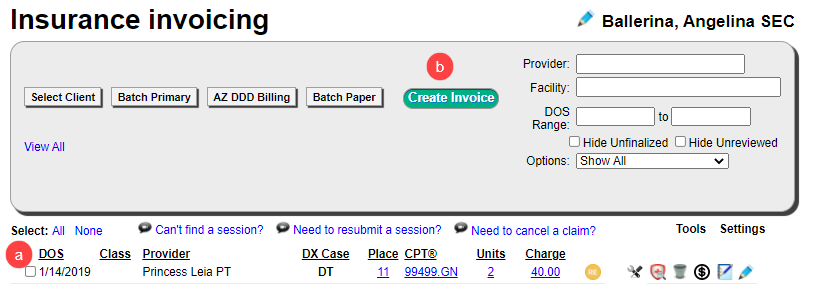
- From the Billing menu, click Bill Insurance.

- Click Select Client.
- Use the Select Client filter to find the patient session.
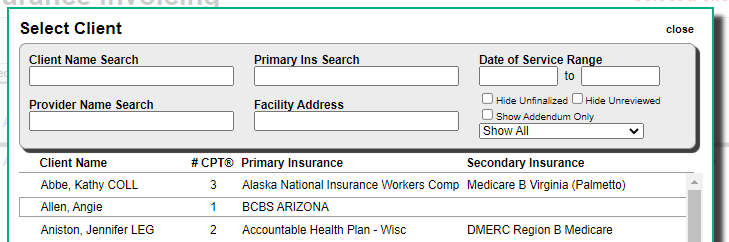
- Check the session (a) and click Create Invoice (b).
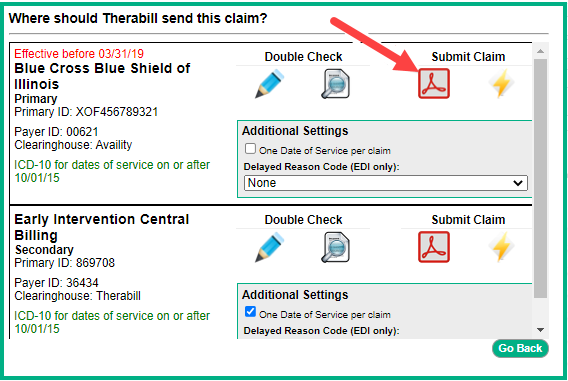
- Click the PDF icon for the appropriate insurance payer as though you were to submit a claim by mail.
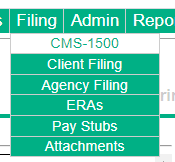
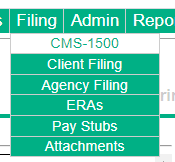
- Once the claim is generated by PDF click the Filing menu, then click CMS 1500.
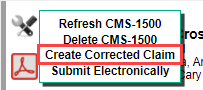
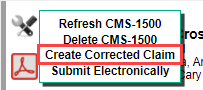
- Click the tool icon.
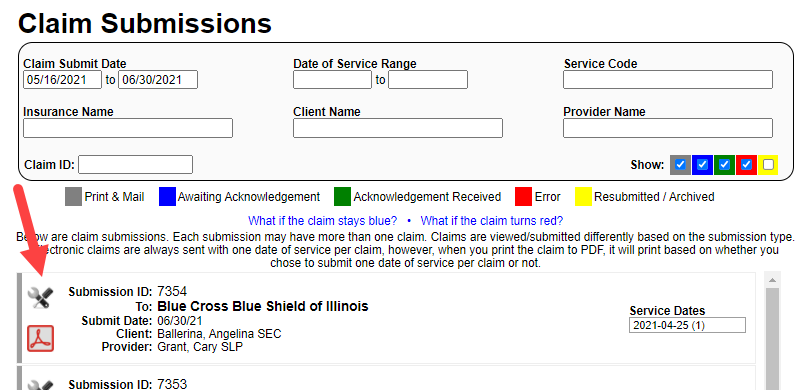
- Select Create Corrected Claim.
- In Step 1 Select claims, check the boxes that need to be corrected for the claim.
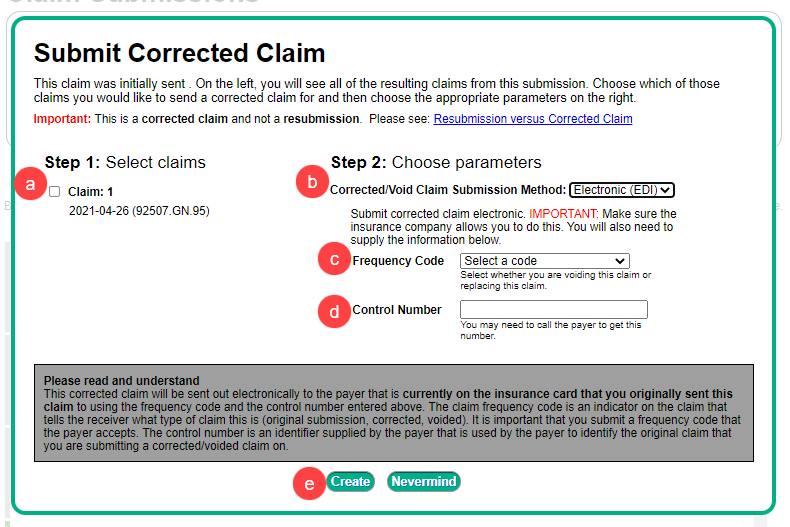
- In Step 2 Choose parameters, choose Electronic EDI from the Corrected/Void Submission Method drop-down.
- Select Replace submitted claim [7] from the Frequency Code drop-down.
- Fill in the Control Number received from the Payer. This can often be found on the EOB or ERA, otherwise, you will need to contact the Payer to obtain the control number.
- Click Create
- In Step 1 Select claims, check the boxes that need to be corrected for the claim.
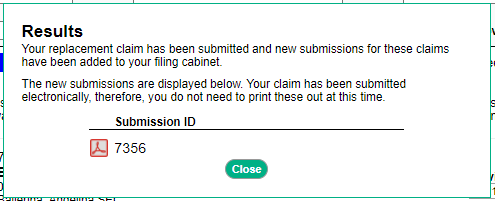
- The new submission will be created in the CMS-1500 File Cabinet for each claim selected in Step.
Printed/Mailed Corrected Claims
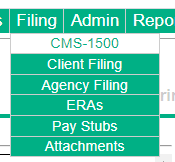
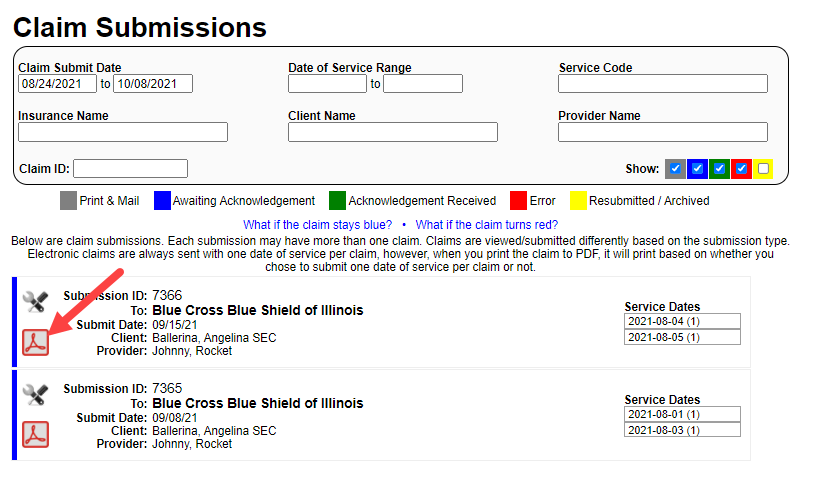
- Find the claim in the CMS-1500 File cabinet, click the Filing menu, then click CMS 1500.
- Click the tool icon
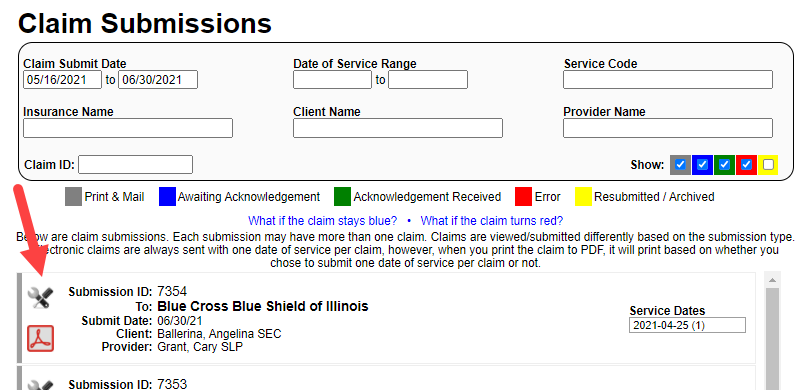
- Select Create Corrected Claim.
- In Step 1 Select claims, check the boxes that need to be corrected for the claim.
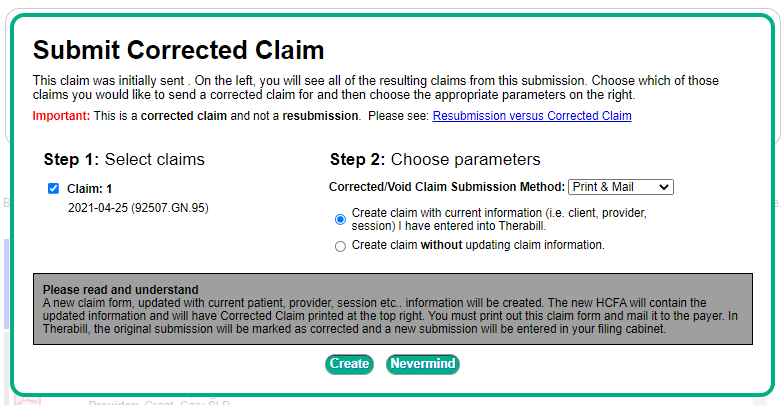
- Step 2 Choose parameters, choose Print & Mail from the Corrected/Void Submission Method
- Drop-down, and choose to Create claim with current Information or Create claim without updating claim information. Either option will print Corrected Claim in the top right.
- Click Create.
- Click the Filing menu, then click CMS 1500 to open the new submission in the CMS-1500 File cabinet.
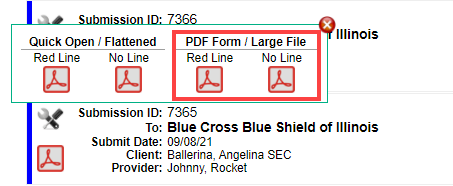
- Click on the PDF icon associated with the new submission.
- Click one of the large file options.
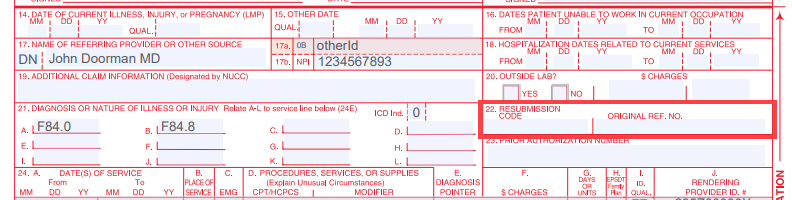
- Enter the Frequency code and control number in box 22.
- Then click Ignore Error on the EDI Rejection to remove the error from the list.

Comments
0 comments
Article is closed for comments.