Although very uncommon, some payers require additional information about the Rendering Provider. The payer (typically Medicaid) may ask for the NTE segment of Loop 2300 to be filled out in order to substantiate the medical treatment when it is not supported elsewhere within the claim. This is called a Claim Note.
Note: Adding a Claim Note that has not been deemed necessary may result in a claim rejection.
Set Up
- Navigate to Provider > Provider List.
- Edit the desired provider using the corresponding
 icon.
icon. - Select the Clm NTE tab.
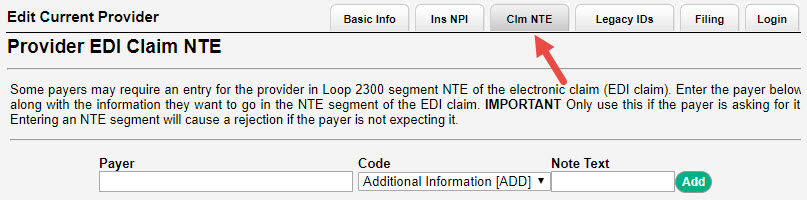
- Enter the Payer name and select them from the drop-down list.
- Use the Code drop-down to indicate ADD or CER as directed by the payer.
- Enter the Claim Note text.
- Select Add. The information will be displayed under Current Claim Notes.
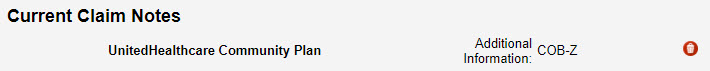
Delete
To remove a Claim Note for a specific insurance, simply select the ![]() icon to the right of the entry.
icon to the right of the entry.
EDI File
Loop 2300, Segment NTE01, NTE02

Comments
0 comments
Article is closed for comments.