EDI rejections do occur, so it's important to understand why they happen and how to prevent them in the future.
EDI Processing
When you submit a claim electronically, an 837 EDI claim submission file is created and sent through the clearinghouse to the payer. While the application completes a basic error check before the claim is sent, every payer has their own requirements for EDI claim. Both the clearinghouse and the payer's EDI department will scrub the claim looking for errors.
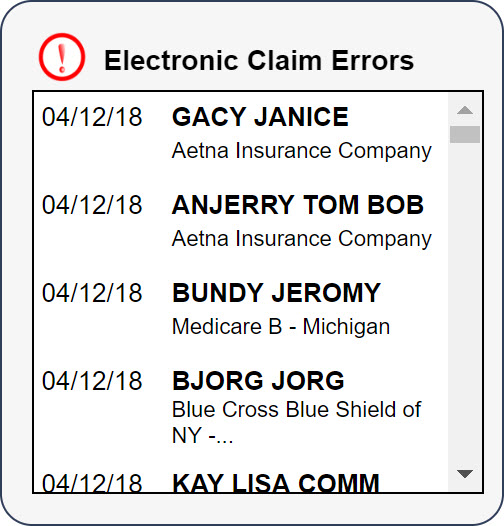
If an error is found, an error file is sent back to our system. Once received, a link to the error will be generated under the Electronic Claim Errors section of the dashboard.
EDI Rejection Page
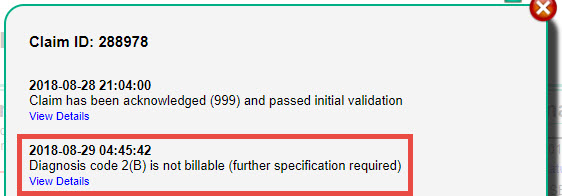
The EDI Rejection page shows what error message(s) were received. The system will try to match the error to a knowledge base article that provides an explanation of the error and how to correct it. These articles can also be found in the Electronic Claim Errors Knowledge Base.
Call the Clearinghouse or Payer
If there is no related article or if you still are not sure how to correct the error, you will need to contact Jopari or the Payer’s EDI department to identify the reason for the rejection. If the payer is unable to locate the claim, please reach out to Therabill Support at 866-221-1870 option 2. In order to determine which entity to call, you will need to locate the Payer Reference Number.
Locate Payer Reference Number
- From the EDI Rejection screen, locate the Edit Claim Information box.
- Select the View Status Messages link. A new window will appear.
- Messages received from the clearinghouse and payer will be listed in ascending order, with the most recent at the bottom. Locate the most recent entry and select View Details. A .txt file will be downloaded to your computer.
- When you open the file, there will be a lot of information that appears to be incoherent. Feel free to copy and paste the data into a word processing application (i.e. Microsoft Word). This might make it easier to locate the needed fields.
- To contact the Payer’s EDI department, pinpoint the [PAYER_REF] item. If there is an entry for this field, you will know that the claim made it to the payer and that you should contact them. The number located in this field is the Payer Claim Reference Number, you'll need to provide this information to the payer to discuss the rejection with them. If the [PAYER_REF] field is blank, the payer may still be able to locate the claim with the patient’s information and date of service. If they are unable to locate the claim, contact Therabill Support.
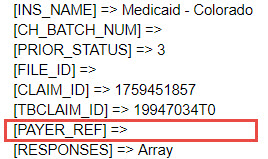 Note: If claims go through Jopari you will not need to locate the PAYER_REF. Refer to the next step below on contacting the Clearinghouse.
Note: If claims go through Jopari you will not need to locate the PAYER_REF. Refer to the next step below on contacting the Clearinghouse. - To contact the Clearinghouse, find the [CLEARINGHOUSE] item. You can determine which Clearhouse it was sent to within this file. If the claim was sent to Jopari, provide them with the Client's Name, Date of Service, and your Jopari Username for assistance.
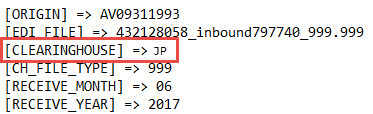
- AV: Availity
- JP: Jopari
If you are given information about what loop and segment the error is located in, you can find more information on correcting those errors here: EDI (837) Files.
| Therabill Support | Jopari | |
| Phone Number | 866-221-1870 | 800-630-3060 |
| Phone Prompt | Option 2 |
Resubmission vs. Corrected Claims
If the claim was rejected, you can typically resubmit the claim as new, because it was never accepted by the payer for adjudication. For more information, please see: Resubmission vs. Corrected Claim.
Note: If you need to make any demographic changes, they should be updated in WebPT as well.

Comments
0 comments
Article is closed for comments.