An Electronic Data Interchange (EDI) file is the electronic version of a CMS-1500 form.
An EDI file is sent after creating a claim, representing the outgoing communication of the insurance billing process. This 837 file (the technical term for an EDI claims) needs to be routed through a clearinghouse to ensure it arrives at the correct destination. EDI is also how payers and clearinghouses communicate with your clinic to acknowledge receival of a claim or to send a claim rejection message.
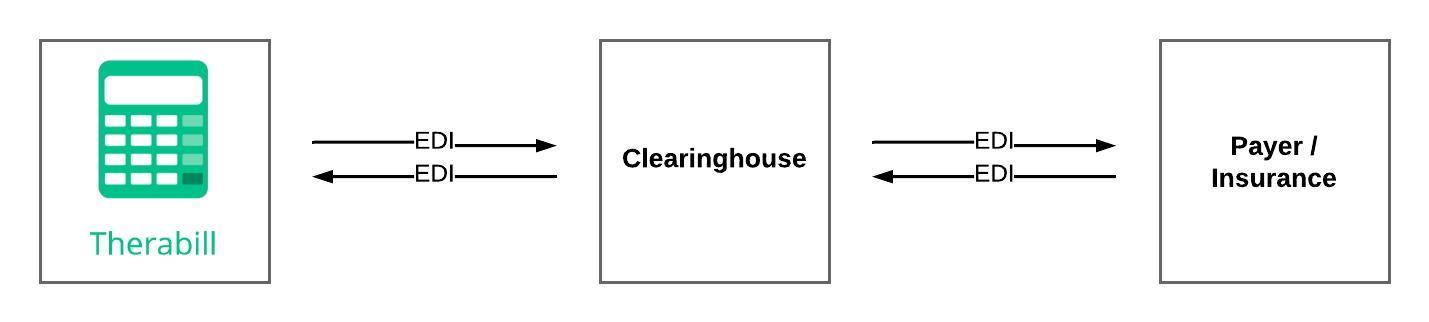
Clearinghouses
Clearinghouses act as the go-between for billers (your clinic) and payers (the insurance company). In order to create an easier and more seamless experience, we have established our own account with each clearinghouse. Therefore, you do not need to create your own clearinghouse accounts, which reduces extraneous steps and paperwork. We use the following clearinghouses:
- Availity
- Jopari (Auto & Workers Comp)
An extremely important part of this process is the Electronic Payer ID. This payer identification number is what allows the clearinghouse to route the EDI file to the right payer. If a payer is not receiving your EDI files, ensure that your Electronic Payer Identification number has been entered correctly.
EDI Enrollment
EDI enrollment is the process required by some insurance companies to begin accepting electronic claims from a clinic. Until your clinic has enrolled and received approval from the insurance company, the system will not allow you to send out claims electronically.
For more information, please see: EDI & ERA Enrollment Guide.
For Jopari, please see: Jopari Clearinghouse
Electronic Remittance Advice (ERA)
An Electronic Remittance Advice (ERA) is the electronic version of an Explanation of Benefits (EOB). These are also known as 835 files. Just as your electronic claims (EDI) are routed through a clearinghouse, your ERAs are too. The system is simply a receiver of information (think of a mailbox). Therefore, any ERA enrollment questions or issues will have to be addressed by the sender (insurance company) or the clearinghouse (think of the post office).
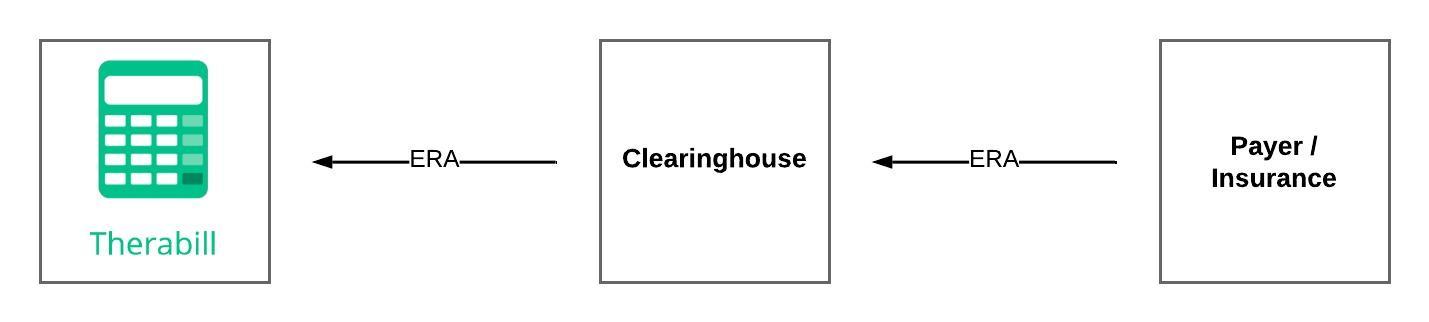
Important: An ERA is an explanation of the funds that a payer has issued to you. The actual funds are never sent through, or handled by, the system.
ERA Enrollment
ERA enrollment is the process required by all insurance companies to begin receiving electronic remittances from a payer. Until your clinic has enrolled and received approval from the insurance company, you will receive paper EOBs.
For more information, please see: EDI & ERA Enrollment Guide.
Note: Not all insurance companies provide ERAs. For those that do, ERA enrollment is required.
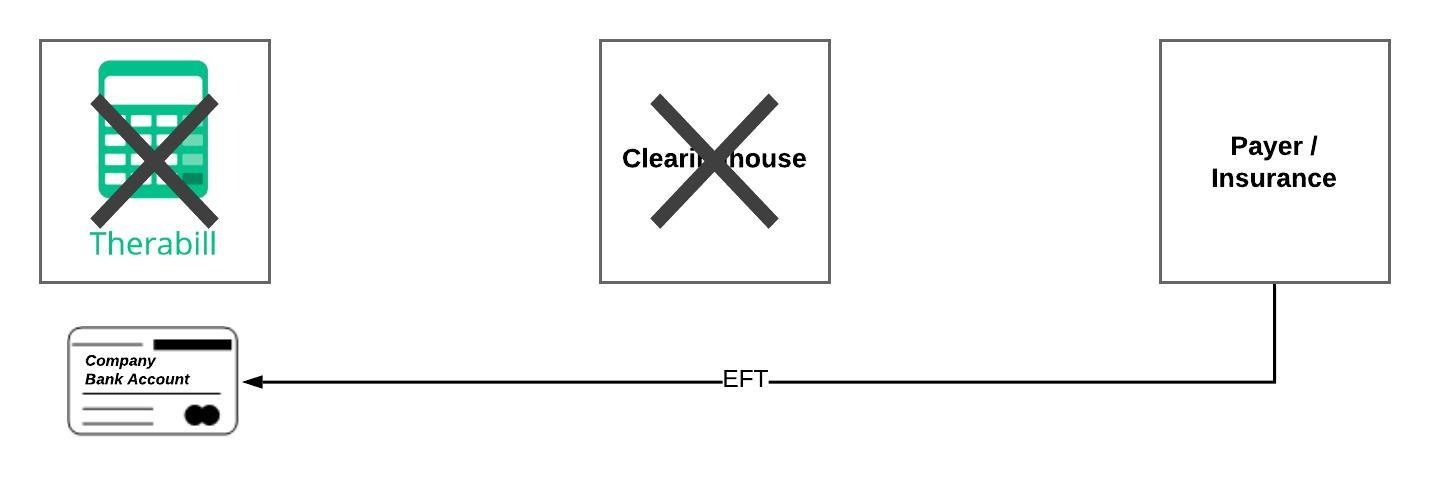
Electronic Funds Transfer (EFT)
EFT is the process of an insurance company sending payment from their bank account directly to yours. Your payment for services will never pass through a clearinghouse or the application. If there is ever an issue with a delayed, missing, or incorrect payment, you will have to contact the payer.
FAQs
If I’m enrolled for EDI (electronic billing) or EFT (direct deposit), does that mean I’m enrolled for ERA?
No, it's more common for the enrollments to be separate and unrelated. You can be enrolled for none, one, two, or all options with each insurance company. Typically one enrollment has no impact on the other, so do not assume enrolling for one enrolls you for others.
ERA Payment Posting
For more information, please see: ERA Payment Posting.

Comments
0 comments
Article is closed for comments.