ERA Enrollment
ERA (Electronic Remittance Advice) is the electronic version of an EOB (Explanation of Benefits). It is common for an insurance company to send a check and EOB when they pay a claim. The EOB explains what payments are included in the check.
For easy and efficient billing, Therabill allows you to have the ERA sent directly to your Therabill account. To use this feature, ERA enrollment and approval are required for any payers that offer ERAs.
EDI Enrollment
In addition, some payers require Electronic Data Interchange (EDI) approval for a clinic to submit claims electronically.
What if I am not enrolled?
- The payer will not accept any submitted ERA claims if EDI approval is required and a clinic does not enroll.
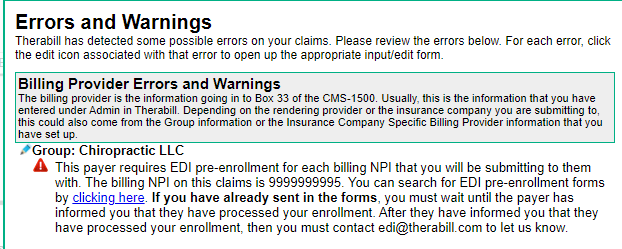
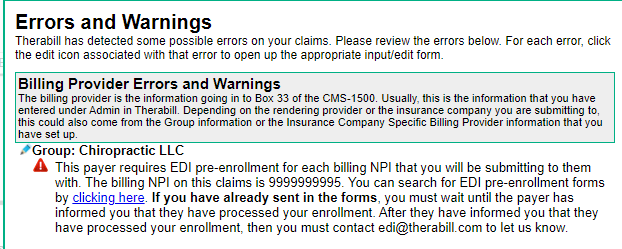
- The following warning will display if a payer requires EDI enrollment and you are not yet enrolled. You will need to complete an EDI enrollment or bill these claims out as print & mail claims.
Process
Your initial Availity EDI/ERA enrollment is handled by your Onboarding Specialist when your Therabill account is set up. To add a new insurance company to the list of EDI and ERA enrollments after your onboarding is complete contact Therabill Support by email Support@Therabill.com or by phone at 866-221-1870 option #2 for Support and #2 Therabill.
Please have the following required information available to complete additional enrollments:
- Payer Name & Payer ID
- Billing NPI (indicate Group or Individual)
- Tax ID
- PTAN (Medicare Only)
- Provider/Legacy ID Number (for Medicaid Only)
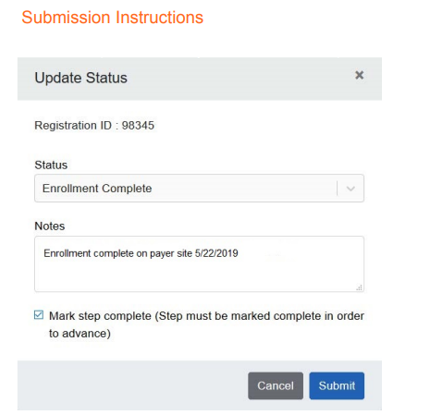
Your Support Specialist will submit the enrollment request to Availity on behalf of the clinic and provide additional enrollment instructions via your Therabill account.
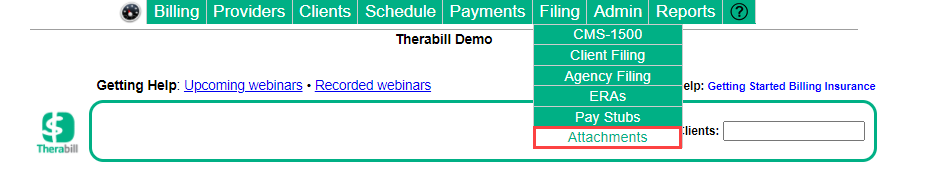
- To access these instructions and complete your enrollment forms, go to Filing > Attachments.
- Follow the instructions to complete and submit the forms. Depending on the enrollment you may need to download and print the forms or you will be instructed to follow a hyperlink to complete the instructions electronically. Note: If you have additional questions regarding completing these forms use the contact information provided on the forms.
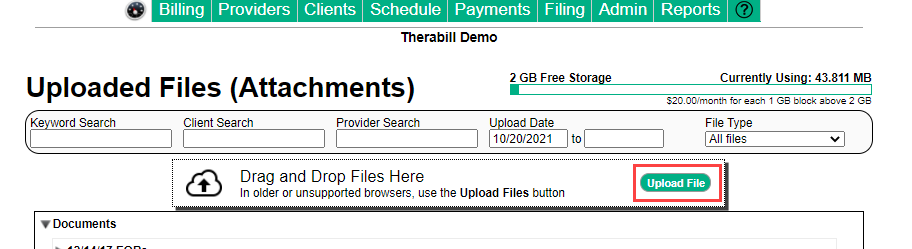
- Once the forms are complete, upload a copy to your Therabill account. Go to Filing> Attachments and click Upload File.
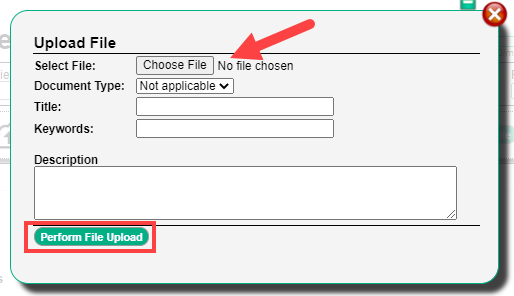
- Choose the file from your computer, complete or review then click Perform File Upload.
- After you send the completed forms to the payer, contact Therabill Support to submit the completed forms to Availity. Please include your Group NPI, this allows the Therabill support team to complete the Submission Instructions.
EDI Enrollment Process
Some claims for the designated payer will display an EDI Approval warning after submitting the EDI enrollment forms, contact Therabill Support to request EDI Approval.
Please include:
- Group NPI
- Payer name/Payer ID
- Submitter ID - The Submitter ID sequence is usually seven characters and includes the state initials.
FAQs
How do I check the status of my enrollment?
It can take up to six weeks for a payer to approve your enrollment status. If you have submitted all your paperwork to the payer and submitted your completed enrollment forms through Therabill (see submission instructions), contact the payer directly to check the status of your EDI/ERA enrollment. WebPT Therabill does not communicate with payers and will not be made aware of the status.
I’m missing ERAs, what can I do?
Contact the payer when you discover any missing ERAs. The payer may request that you resend the files. If the payer confirms the files were sent to Availity, contact Therabill Support and provide the payer’s name, payer ID, check date, check number, and check amount. Note: For files over 15 days old, pull the EOBs from provider portals and manually post.
https://therabill.zendesk.com/hc/en-us/articles/217245463-COB-Batch-Ins-Payment-Entry

Comments
0 comments
Article is closed for comments.