In March 2019, we began to send out communication regarding the clearinghouse upgrade project. Beginning September 1, 2019, all Therabill users will be migrated from the Office Ally clearinghouse to Availity. Please see below for frequently asked questions.
Unable to invoice claims?
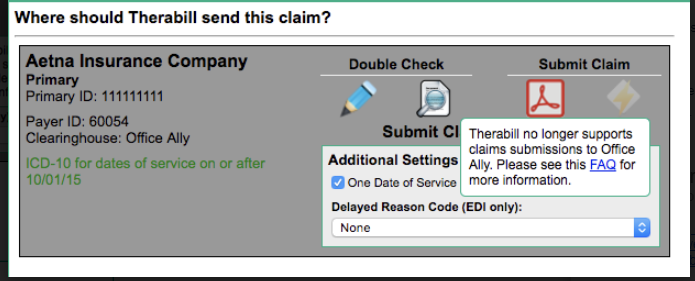
We will not allow any claims submissions to Office Ally as of 9/1/2019. The following error will be displayed when submitting claims for an individual.
If you've already been approved for EDI and your claims are still unable to be invoiced, ensure that the client's insurance card is mapped correctly to an Availity payer.
If you've submitted the enrollment forms, please verify the status with the payer. Let us know immediately if you have approval and we'll update your account.
Claim Rejections
Verify the payer ID you are submitting is accurate, most times this is listed on the insurance card.
If Rejection Message Contains:
- Submitter not approved: Do you have approval to submit to this payer? Please be sure insurance settings match the NPI/TIN/Provider approved for claim submission.
- Subscriber ID being invalid: Please be sure all patient/subscriber information is accurate on demographics and insurance cards. We also recommend verifying benefits with the payer.
- Diagnosis or codes invalid on the session: Please review the CPT or ICD-10 codes to ensure you're following the insurance guidelines with limitations and modifiers.
- Missing/Invalid Other Insured Name (HCFA box 9, UB box 58): Please ensure that your ERAs have been remapped to the Availity payer that matches the client's insurance card.
Are you submitting to a Blue Cross payer that requires the BL plan type? Please read here for more information.
Do you have an approval? Please contact us immediately and we'll make the necessary adjustments within your account.
Do you need to remap an ERA? Type the payer name or payer ID into the "Insurance Company" field on the ERA and click Update Insurance Mapping. 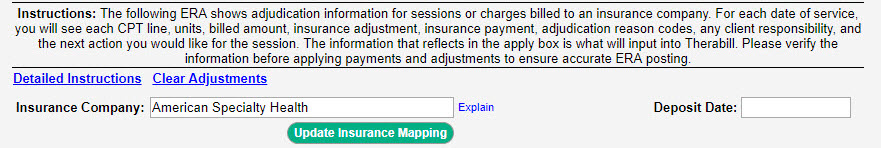
Missing ERAs
If you're missing ERAs, obtain them from the insurance provider portal. Once received, please post them within Therabill using the COB Batch Insurance payment entry form.
If you're currently receiving ERAs and are missing certain dates, please ask the payer to resend them.
If your ERA enrollment has not been processed by the payer, you're not receiving ERAs from Availity, please utilize your insurance provider portals to obtain EOBs.
Claims Invoiced to Office Ally from 9/1-9/4/19
Claims billed to an Office Ally payer from your account between 9/1-9/4/2019, were not transmitted to the clearinghouse and will require action on your part. Click here for instructions.

Comments
0 comments
Article is closed for comments.