Starting January 1st, 2021, Early Intervention (EI) in Illinois now requires that all services rendered by 02-Telehealth have an authorization in Box 23. Review the instructions below to ensure the authorization number appears on your telehealth claim submissions.
In this article, we’ll cover the following scenarios:
- EI is Primary, No Secondary
- Primary Doesn’t Require Auth, EI is Secondary
- Primary Has Combined Benefits Max, EI is Secondary
- Primary and Secondary (EI) Require Authorization
- How do I bill for IFSP development time and meetings if a child has a commercial primary insurance provider?
Scenario 1: EI is Primary, No Secondary
The patient has the following insurance scenario:
- Insurance Cards
- Primary: EI - authorization required
- Secondary: none
- All services are rendered via 02-Telehealth
- EI authorization #: 999-888 must go out on the claim
How to Populate Box 23
Enter an authorization on the client’s account to ensure that the authorization number correctly populates on the claim form.
Scenario 2: Primary Doesn’t Require Auth, EI is Secondary
The patient has the following insurance scenario:
- Insurance Cards
- Primary: BCBS - authorization not required
- Secondary: EI - authorization required
- All services are rendered via 02-Telehealth
- BCBS plan does not require authorization or benefit maximum tracking
- EI authorization #: 999-888 must go out on the claim
How to Populate Box 23
Enter an authorization watch for the EI only. So long as there is no authorization watch tied to the primary, your secondary EI claim will populate the authorization number on the claim form.
Scenario 3: Primary Has Combined Benefits Max, EI is Secondary
The patient has the following insurance scenario:
- Insurance Cards
- Primary: BCBS - has a combined services benefit max
- Secondary: EI - authorization required
- All services are rendered via 02-Telehealth
- BCBS plan has a 60 visit combined maximum for occupational, physical, and speech therapy. This does not require an authorization; however, you will need to track the number of visits applied toward this benefit maximum.
- EI authorization #: 999-888 must go out on the claim.
How to Populate Box 23
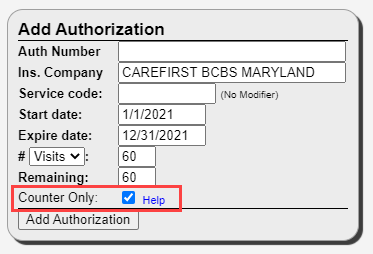
Create an authorization for both BCBS and EI. When you enter the BCBS authorization, be sure to leave the authorization number field blank and check the Counter Only box at the bottom of the authorization. This will ensure that Therabill accurately counts the number of remaining visits.
When it is time to submit your secondary claim to EI, you will need to manually select the EI authorization on the session before submitting the claim to EI to ensure that the EI authorization number appears on the claim form.
Scenario 4: Primary and Secondary (EI) Require Authorization
The patient has the following insurance scenario:
- Insurance Cards
- Primary: BCBS - authorization required
- Secondary: EI - authorization required
- All services are rendered via 02-Telehealth
- BCBS plan covers 25 visits, authorization #: 123123123 must go out on the claim.
- EI authorization #: 999-888 must go out on the claim.
How to Populate Box 23
Since only one authorization number can be attached to a session, members will need to delete the BCBS authorization from the session, then manually select the EI authorization before submitting the secondary claim to EI. This is the only way to force the EI authorization number to appear on the claim form.
How do I bill for IFSP development time and meetings if a child has a commercial primary insurance provider?
Create an authorization for the IFSP development time or meeting (CPT® code: 99499). Do not include the modifier.
Next, change the Responsibility for your Early Intervention insurance card from Secondary to Primary. When you submit your claim, the authorization number will populate on your claim form. Be sure to change the Responsibility on your Early Intervention insurance card back to Secondary before submitting claims to the commercial primary insurance card on file.

Comments
0 comments
Please sign in to leave a comment.